A-Z of Public Health Topics
Buruli ulcer


Buruli ulcer is an infection of skin and soft tissue caused by the bacterium Mycobacterium ulcerans.
The toxins made by the bacteria destroy skin cells, small blood vessels and the fat under the skin, which causes ulceration and skin loss. Some people have a raised, red lesion called a plaque. The damage caused can be serious and extensive if diagnosis is delayed. Since the ulcer gets bigger with time, early detection, diagnosis and prompt treatment can minimise skin loss and other health harms from Buruli ulcer.
There is strong evidence that mosquitoes and possums play a role in transmitting the infection in Victoria.
Who is at risk?
Cases of Buruli ulcer have increased in Victoria in recent years. The disease is spreading into new geographical areas including these six suburbs in the Western Public Health Unit catchment:
- Brunswick West
- Coburg
- Essendon
- Moonee Ponds
- Pascoe Vale South
- Strathmore.
How does Buruli ulcer spread?
Local research has confirmed that Buruli ulcer is transmitted from possums to people via mosquitoes. The type of mosquitoes that are pests in backyards – especially the common container breeding mosquito Aedes notoscriptus – are the main risk. Reducing mosquitoes on your own property will reduce your risk of infection.
Buruli ulcer can take many months to develop after exposure. People are most often exposed during the main mosquito season, which runs from early November to late April. It then usually takes between 4-5 months to develop Buruli ulcer after a bite by an infected mosquito. This means that often people develop the ulcer in winter or spring after the mosquito season is over. Recognising Buruli ulcer can be difficult but the infection should be considered when a skin lesion relentlessly progresses over time despite standard treatment.
The importance of an early diagnosis
Once diagnosed, Buruli ulcer can be cured with a specific type of antibiotics. It is important to get a diagnosis from a doctor as early as possible. If diagnosis is delayed the ulcer can become very large. The ulcer can sometimes lead to deformity, disability, or bone infection.
How to recognise Buruli ulcer
- Buruli ulcer may start like a bite or as a lump under the skin that gets bigger over days or weeks.
- Buruli ulcer occurs on areas of the body where mosquitoes bite, including the ankle, lower leg and arms.
- Unlike other ulcers, Buruli ulcer often does not hurt. Usually, people do not have fever or other symptoms of infection.
What to do if you have a new or persistent sore, ulcer or skin infection
See your GP. Ask about getting an easy Buruli ulcer test.
Preventing Buruli ulcer
Reduce the number of mosquitoes around your property:
- remove or cover any source where mosquitos breed with mosquito wire, such as gutters, pot plant containers, buckets, open tins or cans. Empty out stagnant water
- make sure your water tank is screened off to prevent mosquitoes from breeding there
- mosquito proof your home by installing insect screens.
Avoid mosquito bites:
- use personal insect repellents containing diethyltoluamide (DEET) or picaridin
- cover up by wearing long, loose-fitting, light-coloured clothing
- avoid mosquito-prone areas especially at dusk and dawn when they are most likely to be out.

Reducing your risk of mosquito bites, especially during mosquito season (early November to late April) and especially around your own property, can greatly reduce your risk of Buruli ulcer.
For more information on protecting yourself from mosquito bites, click here.
Professor Paul Johnson is an Infectious Diseases Physician who for 30 years has led or co-led Buruli ulcer research in Victoria and has extensive clinical experience with Buruli ulcer.
For more information about Professor Paul Johnson, view his website here.
Buruli ulcer information for health professionals
Cases of Buruli ulcer have increased significantly in Victoria in recent years. The disease is spreading into new geographical areas and Western Public Health Unit has identified a localised outbreak of Buruli ulcer in six suburbs in the WPHU catchment. These are:
- Brunswick West
- Coburg
- Essendon
- Moonee Ponds
- Pascoe Vale South
- Strathmore.
Buruli ulcer is an infection of skin and soft tissue caused by the bacterium Mycobacterium ulcerans. The toxins made by the bacteria destroy skin cells, small blood vessels and the fat under the skin. Ulcers appear as the infection spreads in the fat layer beneath the skin. The damage caused can be serious and extensive if diagnosis is delayed.
Local research has confirmed that Buruli ulcer is transmitted from possums to people via mosquitoes. The type of mosquitoes that are pests in backyards – especially the common container-breeding mosquito Aedes notoscriptus – are the main risk. Reducing mosquitoes on your own property will reduce your risk of infection.
The median incubation period is 4-5 months with a range of 1-10 months. Often ulcers appear 4-5 months after mosquito season (early November to late April) and present to care or are diagnosed in winter or spring.
Generally, 80-90 per cent of cases have an ulcer, while some others have relatively slowly progressing cellulitis that does not respond to standard treatment. Consider Buruli ulcer in patients with an ulcer who might have exposure in an area of risk.
Testing
Test ulcers for M. ulcerans by taking a swab from the undermined inside of the edge of an ulcer, ensuring you can see biological material on the swab. It is important to specifically request M. ulcerans smear, culture and PCR as laboratories will not routinely do these tests.
If there is a plaque with no ulcer, a punch biopsy that samples the subcutaneous layer will be required.
Treatment
Treatment is generally with rifampicin and clarithromycin for 8 weeks. Local infectious diseases specialists and hospital clinics are happy to support GPs to treat patients or to initially manage patients as they are commenced on antibiotics. Dressings may be required for weeks after antibiotics are completed. Surgery is reserved for specific situations and is not usually required.
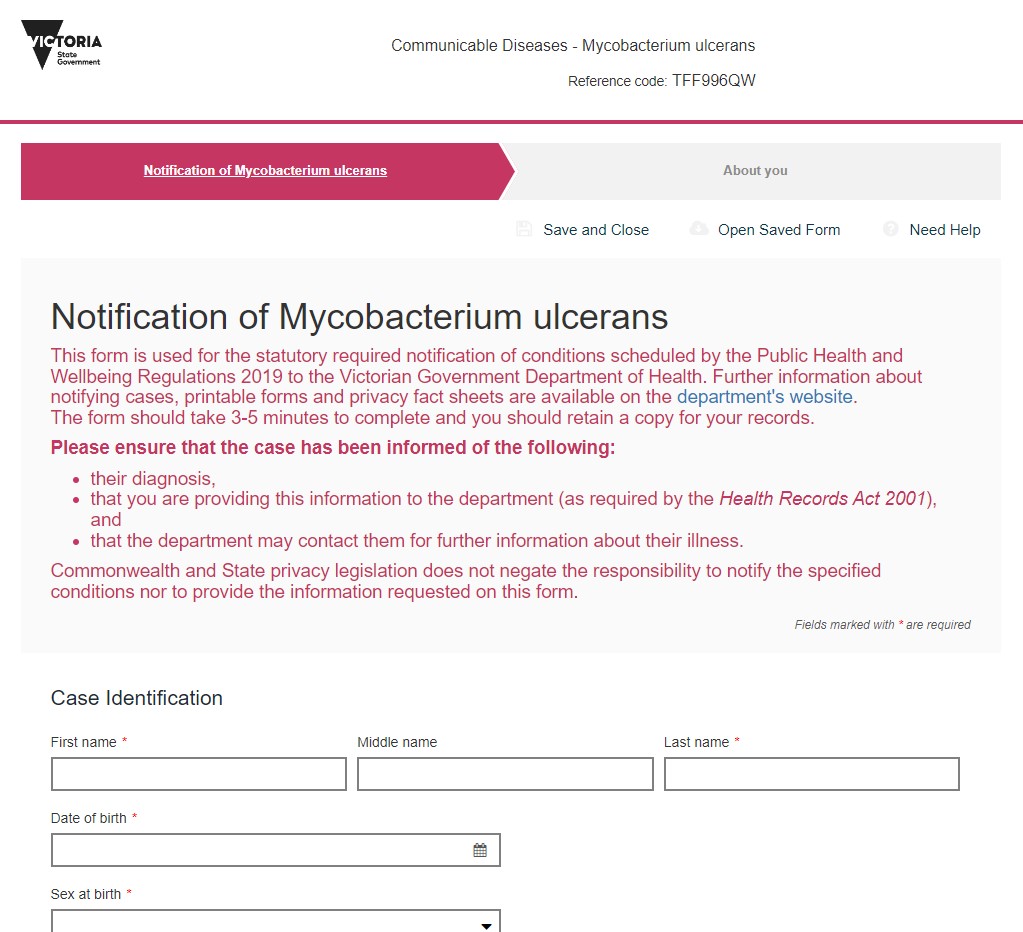
Notification
Mycobacterium ulcerans infection is a notifiable disease in Victoria under the Public Health and Wellbeing Act 2008. Clinicians must notify all confirmed cases, which can be done by completing the online notification form.
Resources
See this useful summary for further information about identification, testing and treatment of Buruli ulcer.
Professor Paul Johnson is an Infectious Diseases Physician who for 30 years has led or co-led Buruli research teams in Victoria. Paul has extensive clinical experience with Buruli ulcer and developed the first Australian Buruli Consensus treatment guidelines in 2007 which have since been updated. Paul has also been a member of the WHO Technical Advisory Group on Buruli ulcer since 1998.
For more information about Professor Paul Johnson, view his website here.
